What are the advantages of living donor liver transplantation?
The main advantage of living donor liver transplantation is that the recipient can undergo the transplant when needed, without having to wait for their turn on the cadaveric transplant waiting list. Since organ donation rates are extremely low in our country, patients on the list may experience worsening health or even lose their lives while waiting for a suitable organ. Additionally, a patient’s overall condition may deteriorate during the waiting period, increasing the risk of postoperative complications and decreasing the likelihood of success after transplantation. If there were a sufficient number of cadaveric livers available, living donor transplantation would not be considered as frequently.
How much of the donor’s liver is removed?
Generally, between 40% and 70% of the liver is removed. The liver is divided into two parts — the right and left lobes. This natural anatomical division allows surgeons to obtain two separate liver portions that can function independently. The right lobe makes up approximately 60% of the liver, while the left lobe accounts for about 40%. During the transplantation surgery, the donor’s gallbladder is also removed.
How much time should pass between removing the liver from the donor and transplanting it into the recipient?
The donor and recipient surgeries are performed simultaneously.
Can anyone be a living donor?
In general, to be a donor, you must be between 18 and 55 years of age.
It is preferable for the donor and recipient to be of similar body size. If the donor is female, she should not be pregnant. The donor should not be overweight; however, if overweight, they may still become a potential donor after losing weight. The donor must be completely healthy. They must also fully understand all the risks associated with this surgery and be willing to comply with all medical instructions given by the doctors in both the short and long term after the operation.
Does the donor have to be related to the recipient?
In our country, individuals up to the fourth degree of kinship can be liver donors. Donors who are not related to the recipient are evaluated and approved by the Ethics Committee of the Ministry of Health.
If I am related to the recipient, does that reduce the risk of rejection?
Studies have shown that a genetic relationship between the donor and the recipient does not reduce the risk of rejection. Additionally, the relationship between the donor and the recipient does not affect the level of immunosuppressive therapy required by the recipient after surgery. However, identical twins may present an exception in such cases.
What is evaluated during the assessment process?
The donor and recipient must have compatible blood types. During the evaluation, it is checked whether the donor’s liver is healthy and of adequate size. It is also ensured that the donor does not have any psychiatric condition that could complicate the procedure. The donor must be free of any infectious diseases that could be transmitted to the recipient. Finally, the donor must have made the decision voluntarily and without any external pressure.
Can I have the evaluation done by my own doctor?
Since organ transplantation is a detailed process, it is best for all tests and evaluations to be performed by our team. However, if you live far from our center, part of the evaluation may be done locally where you live, but in all cases, you will need to be reviewed by our doctors.
What is the first step of the evaluation?
The first step in the evaluation is to determine your blood type. This is a very simple test that can be done by your doctor or at any blood center. The donor’s blood type must either be the same as the recipient’s or type “O.” The Rh factor (+ or −) of the donor has no effect.
If I already know my blood type, what should I do?
You can call our transplant center and speak with our transplant coordinator.
You may ask any questions you have over the phone. Your detailed personal information will be collected, and an appointment will be scheduled for a suitable time. During your appointment, your medical history will be reviewed, and a thorough physical examination will be conducted. The physician in charge will inform you about living donor liver transplantation, explaining the risks of the procedure and providing statistical data from our center and worldwide. A comprehensive blood test will also be performed during this visit. After reviewing your results, if everything is satisfactory, the second step of the process will be planned.
What is the second step in the evaluation?
The next step in the evaluation is a detailed radiological examination. The size and blood supply of your liver are measured. A CT scan provides detailed information about your liver and plays a major role in the decision-making process. In addition, a hepatologist and a surgeon from our team will evaluate you. Other tests may also become important depending on your specific condition.
Should I fast before coming to my appointments?
You should fast for 3–4 hours before the CT scan and 8 hours before the MRCP. However, unless you are specifically instructed otherwise, you do not need to come to your appointments fasting.
Should my family accompany me to the appointments?
It is important to have a relative or family member accompany you to your appointments. This way, they can also become informed about the procedure. During these visits, both the donor and their family can ask any questions they have and obtain more information. It is recommended that your accompanying family member stay with you until the final appointment.
| Blood Type | Can Receive From | Can Donate To |
|---|
| O |
O |
O - A - B - AB |
| A |
O - A |
A - AB |
| B |
O - B |
B - AB |
| AB |
O - A - B - AB |
AB |
When will I find out if I can be a donor?
Genel olarak değerlendirmeyi bitirdikten hemen sonra bilgilendirilirsiniz. Bazen ameliyatınızı etkileyeceği düşünülen ileri tıbbi testlere ihtiyaç duyulabilir. Size verilen bilgileri anlamış olmanız son derece önemlidir. Karaciğeriniz bağışlama kararı ciddi bir karardır.
Who makes the final decision on whether I can be a donor?
After all the necessary tests have been completed, our team will meet to review the results. Our team includes doctors, surgeons, nurse coordinators, radiologists, anesthesiologists, psychiatrists, and, if applicable, consulting physicians who evaluated you during your appointments. The final decision is never made by an individual; it is always made collectively by the team. The donor’s health is always the primary consideration in this decision.
Who decides the transplant date once I am confirmed as a donor?
The transplant date is determined jointly by the surgical team, the recipient, and the donor.
Depending on the recipient’s condition, doctors may prefer to perform the surgery as soon as possible. In such cases, discussions are held with the donor, and surgical preparations begin. Operating room coordination is also crucial. The transplant requires two operating rooms and two full teams consisting of surgeons, nurses, and anesthesiologists.
Should the cause of the recipient’s illness affect my decision?
The donor volunteers to make a great sacrifice by giving a portion of their liver. This act of generosity will save the recipient’s life. Some diseases, such as hepatitis C and liver cancer, may recur after the transplant. Before the surgery, what can be expected from the transplant, possible complications, and the recipient’s current medical condition will be discussed with you. Confidentiality is essential in these discussions, and the same sensitivity is expected from the donor. These matters will not be hidden from the recipient.
What are the possible complications of the donor surgery?
The risk of death in donor surgeries is 0.2%, which is a very low rate.
There is a potential risk of bleeding and bile leakage after the surgery. These situations may rarely require a blood transfusion or a second operation. Although the occurrence of such complications is quite rare, the risk always exists. These risks will be explained to you in detail during the evaluation process. Minor bile leaks, small wound infections, and some gastrointestinal issues (such as constipation, indigestion, and nausea) are the most common complications. These complications typically resolve within a few weeks.
Is the gallbladder removed during the surgery?
The gallbladder is removed during the liver transplant surgery. This has no negative impact on the donor’s health or quality of life afterward.
Will I receive a blood transfusion during my surgery?
Although it is very rare, a blood transfusion may occasionally be required for the donor.
Should I stop consuming alcohol?
If you are going to be a liver donor, it is best that you avoid consuming alcohol. If you have a history of heavy alcohol use, you must inform your doctor. Having consumed alcohol in the past does not prevent you from being a donor; however, a liver biopsy may be required to check whether there is any damage to your liver.
Should I stop taking my medications before the evaluation or surgery?
Do not stop taking your medications unless instructed by your doctors. Aspirin and similar medications should be discontinued 7 days before a liver biopsy or surgery. These types of drugs increase the risk of bleeding complications because they prevent blood clotting. Women who are taking birth control pills or hormone replacement therapy are also advised to stop these medications, as they can increase the risk of postoperative complications by promoting blood clot formation.
How long will I be away from work?
The minimum recovery period after surgery is 4–6 weeks. Since the healing process varies from person to person, it may take 8–12 weeks for pain and fatigue to completely subside.
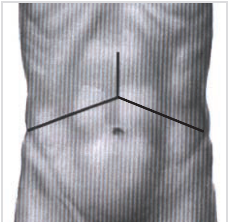
How large is the surgical incision?
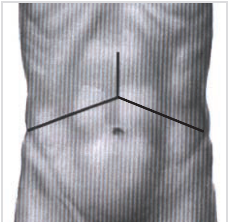
The surgical incision may be J-shaped, a straight incision along the midline, or in the shape of a Mercedes symbol. (See image)
Will there be a scar on my body after the incision heals?
In most cases, the incision heals quickly and gradually becomes smaller; however, it will always remain slightly visible. If the wound becomes infected, the resulting scar may be larger and more noticeable.
Will I experience a lot of pain after the surgery?
During the first three days after surgery, your pain is managed with an epidural catheter. After that, oral medications are used to control your pain.
Will I have a normal life after the surgery?
If no complications occur, you can expect to return to your normal life in about three months. The risk of experiencing complications in the long term is very low.
When can I resume my sexual life?
For a few weeks, you’ll probably not want to resume your sexual life until you regain your strength. What really matters is how you feel in terms of comfort and energy.
If I plan to start a family, how long should I wait after the surgery before getting pregnant?
There is no definite answer to this question, but it is recommended that you avoid becoming pregnant for at least 6 months after the surgery.
When can I resume my birth control or hormone replacement therapy?
We recommend waiting at least three months after the surgery before resuming them.
When will my liver return to its normal size?
The liver begins to regenerate immediately. The most intensive regeneration occurs within the first two weeks. By the end of three months, the liver reaches its previous size or close to it.
Will I be able to donate part of my liver to someone else again in the future?
No. Once you have donated a portion of your liver, you cannot donate it a second time.
When can I drive after the surgery?
It is recommended that you avoid driving for four weeks after the surgery. Before deciding to drive, you should feel physically and mentally well, have good reflexes, and most importantly, be free of any abdominal discomfort.
When can I start exercising?
You will actually begin “exercising” as soon as you wake up from anesthesia. You will be asked to perform breathing and coughing exercises, as well as to periodically tense and relax the muscles in your legs. Within 24–48 hours after the surgery, you will be helped out of bed to start walking. Walking plays a major role in recovery. Getting on your feet as soon as possible reduces the risk of many postoperative complications such as blood clots, pneumonia, and muscle loss. A walking program will be prepared for you to follow at home. Remember, the goal is to regain your previous health within 2–3 months.
When can I start strenuous activities such as running, swimming, or weightlifting?
During the first six weeks, you should be careful not to lift anything heavy until your abdominal wall heals. Avoid lifting more than 5 kg. After 6–8 weeks, if you feel well and have no complications, you can return to your normal daily activities, including sports such as running, swimming, aerobics, and cycling. Be very cautious with abdominal exercises—start slowly and increase your strength and endurance gradually with a few repetitions.
When can I travel or fly on an airplane?
Do not make any plans to travel abroad for at least 4 weeks, preferably 8–12 weeks. If you live outside Istanbul and wish to return home, you may do so 2–4 weeks after surgery if you feel well and if there is a doctor in your city who is familiar with living donor liver transplantation and can follow up on your recovery. Please note that if there is even the slightest suspicion of a complication, you will be asked to return to our center for evaluation and treatment. By the end of the 12th week, you can travel anywhere you wish, in any way you prefer.
When a liver transplant is scheduled, does it definitely take place?
Unfortunately, when it comes to liver transplantation, many factors can change our plans. The recipient’s condition may worsen to a point where transplantation is no longer possible, or the recipient may develop an infection or another condition that needs to be treated before surgery.
How long will I stay in the hospital?
The average hospital stay for donors is about 7–10 days.
Will I share the same room with the recipient?
No, the recipient and the donor are usually kept in separate rooms.
Is the donor kept in the intensive care unit after the surgery?
After the surgery, the donor is kept in the surgical intensive care unit for one night for close monitoring. The next day, once the anesthesia has completely worn off and everything is stable—with no bleeding or other complications—the donor is transferred to the regular ward.
When can I eat and drink after the surgery?
You can start eating and drinking as soon as your bowels begin to function after the surgery. Once you have passed gas, it is safe to start sipping water. If there is no nausea or vomiting while drinking water, you may begin consuming liquids and soft foods. Within two days, you can usually resume a normal diet. Some donors may take a little longer to return to their usual eating habits; the less pain medication is used, the faster the bowels recover.
Are tubes or drains placed in the donor during the surgery?
You may have one or two intravenous lines for administering medications or fluids. One of these lines is also used to deliver pain medication. In addition, a catheter will be placed in your bladder to monitor kidney function. One or two small drainage tubes will be inserted into your abdomen.
The IV lines and urinary catheter are usually removed within 3–4 days, and the abdominal drainage tubes are removed within 6–7 days.
Do I have to return to the hospital for follow-up checkups?
Since this is a major surgery, we will monitor you until we are sure everything is progressing smoothly. You should come to our hospital for a follow-up one week after discharge. You will also be scheduled for a check-up at one month after surgery, and later at the third month and the first year.